
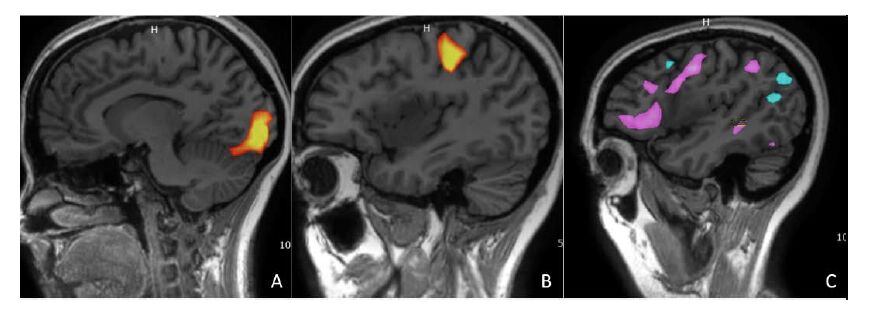
How do you expect the role of high-definition fiber tractography to evolve in the future?Īt the moment high-definition fiber tractography is still a research tool, but we are gaining much more experience. Using this new technology as an aid to surgical planning, patients are getting better, so we are changing the balance of risk and benefit. The expected outcomes for cavernous brain stem malformations are that many patients are worse after surgery. Preliminary data show that we are transforming the outcomes for these patients. By knowing where these fibres are, I can plan a strategy for the safest way to resect the lesion ( Figure 1).
Eloquent brain how to#
The second is that when you reach the lesion, how do you either get through the brain or the exact point where they enter the lesion? Thirdly, once you are dissecting the lesion, how to manipulate the brain tissue around it, which has been compressed or damaged? In the cavity where the lesion is, it is hard to know where the important fibres are. The first is the approach i.e., opening the head. We have taken high-definition fiber technology to a high degree of accuracy, but there are several areas of potential complications with any neurosurgical procedure.

What are the advantages of using high-definition fiber tractography in assessing hyper-eloquent brain lesions? At the University of Pittsburgh, we have advanced this technology so the accuracy is much better and thus have termed it high-definition fiber tractography. Tractography using a technique called diffusion tensor imaging has been available for more than a decade but it has a number of pitfalls, and sometimes is not accurate. High-definition fiber tractography is a technique where data from MRI scanners are processed to reveal the detailed wiring of the brain and to pinpoint fiber tracts. Could you give us a brief description of high-definition fiber tractography? If we knew where these connections were, surgery could be much safer. However, it does not tell us the relationship of the lesion to the other connections in the brain, and this affects our surgical approach. When we look at a magnetic resonance imaging (MRI) scan, it tells us structurally what is around the lesion. What are the limitations of current imaging approaches in assessing whether brain lesions should be resected? However, operating on a more important brain area is more likely to risk neurological complications, so this is a double-edged sword. If you operate on a brain area that is relatively unimportant, you are less likely to have a neurological complication. The term hyper-eloquent is not often used but it refers to particularly important areas of the brain.Ĭonversely, the same risks apply to intervention. A small bleed in a hyper-eloquent area such as the brain stem can have devastating consequences, potentially affecting walking, sense of sensation, causing double vision or death. In an eloquent area, the consequences would be more severe, for example, a small bleed in the motor area might result in an inability to move the arm or leg a bleed in the speech area might leave a patient unable to speak. If the bleed occurs in a part of the brain that is not very eloquent, i.e., there is little clear function, this is not problematic. The risks of not intervening depend on the natural history of the lesion, for example cavernous malformations, a conglomeration of abnormal blood vessels that have variable tendencies to small bleeds. One of the challenges when we see a patient with a lesion that is in, or around, an important part of the brain is to balance the risks and benefits. What are lesions in hyper-eloquent brain and what risks are associated with their resection? 4 In an expert interview, Dr Friedlander discusses the advantages of high-definition fiber tractography, recent advances and exciting potential for the technique in clinical practice. High-definition fiber tractography provides a powerful new tool for imaging nerve fiber connections within the brain, with the potential to improve the accuracy of neurosurgical planning and to advance our understanding of the brain’s structural and functional networks.
1,3 In patients with brain blood vessel malformations, planning the safest approach to surgery is critical. 1 While posing a significant risk of hemorrage, 2 they also present a surgical challenge as the rates of morbidity and mortality are high. Cerebral cavernous malformations are commonly found in deep regions of the brain, such as the thalamus and brainstem.


 0 kommentar(er)
0 kommentar(er)
